Thyroid Cancer

The cancer that arises in the thyroid gland is called thyroid cancer.
Thyroid gland is a small butterfly-shaped gland located at the front,
base of the neck. It secretes hormones such as Thyroxine and
Triiodothyronine, which are useful for digestion, cardiovascular
system, and regulating metabolism, growth, and development.
Thyroid
cancer develops due to various factors that disrupt normal cellular
processes, leading to uncontrolled cell growth in thyroid tissues.
While the exact cause is unclear, several risk factors for the
thyroid cancer have been identified. Most thyroid cancers originate
from follicular epithelial cells, which produce thyroid hormones.
However, medullary thyroid cancer arises from parafollicular C cells,
which produce calcitonin.
Types of Thyroid Cancers
Based
on the origin, behaviour, and histological features TC are
categorised chiefly into five.
-
Papillary
Thyroid Carcinoma (PTC) is the most common type of
thyroid cancer, accounting for 85 per cent of total TC cases. It
arises from the follicular cells of the thyroid gland and is
classified as a differentiated thyroid cancer due to its resemblance
to normal thyroid tissue. It is considered to be slow-developing,
normally confined to the thyroid gland. However, it can also spread
to nearby lymph nodes in the neck, but distant metastases are rare.
Younger individuals and women are most prone to this kind of cancer.
TC
is associated with BRAF and RET/PTC mutations, which contribute to
uncontrolled cell growth. BRAF and RET/PTC regulate cell growth and
division but the mutation of these genes activate Mitogen-Activated
Protein Kinase pathway, which promote abnormal cell growth leading to
PTC.
-
Follicular
Thyroid Carcinoma (FTC) is the second most common
type of thyroid cancer, accounting for 10–15 per cent of cases. It
also arises from follicular cells and is considered differentiated
thyroid cancer. It invades blood vessels more than lymph nodes seen
in PTC. Unlike PTC, it metastasises to lungs, bones, or other
distant sites. FTC mostly associated with iodine deficiency, and
slightly more common in older individuals. -
Medullary
Thyroid Carcinoma (MTC) arises from parafollicular
cells (C-cells), which produce a hormone named calcitonin that
regulates calcium levels in the body. MTC accounts for <5 of
thyroid cancers. This can occur sporadica
-
lly or as part of Multiple
Endocrine Neoplasia type 2 (MEN2) syndromes. Germline or somatic
mutations in the RET proto-oncogene can lead to its constant
activation, resulting in unregulated cell division and tumour
formation. MTC is moderately aggressive, with potential metastasise
to lymph nodes and distant organs like the liver or lungs. -
Anaplastic
Thyroid Carcinoma (ATC) is a rare though highly
aggressive form of thyroid cancer, accounting for about 1–2 per
cent of all thyroid cases. It typically arises from previously
differentiated thyroid cancers, normally in older individuals, and
is characterized by rapid growth and early metastasis to distant
organs. Genetic mutations such as TP53 and TERT promoter mutations
are frequently implicated, disrupting normal cell cycle regulation
and promoting uncontrolled proliferation. ATC presents as a rapidly
enlarging neck mass, accompanied by symptoms like difficulty
breathing or swallowing. Due to its aggressive nature and resistance
to conventional treatments like surgery or radioactive iodine
therapy, the prognosis for ATC is extremely poor, with a median
survival of only a few months. -
Other
rare types of thyroid cancer include Hurthle cell
carcinoma, thyro -
id lymphoma, and thyroid sarcoma. Hurthle cell
carcinoma, a subtype of follicular carcinoma, consists of
oncocytic cells and is more aggressive, with a higher likelihood of
metastasis and recurrence. Thyroid lymphoma arises from
lymphocytes within the thyroid gland, in the context of chronic
autoimmune conditions like Hashimoto’s thyroiditis, and it
typically responds well to chemotherapy and radiation. Thyroid
sarcoma, an exceedingly rare type, originates from connective
tissue within the thyroid and is highly aggressive, with a poor
prognosis. These rare forms of thyroid cancer vary significantly in
behaviour, treatment ap -
proaches, and outcomes, highlighting the
importance of accurate diagnosis for effective management.
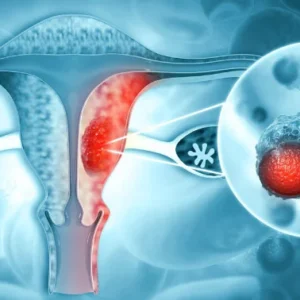
Image
Source: Wikipedia
Symptoms
Thyroid
cancer initially presents with a painless lump in the lower front
part of the neck during initial stage, which is typically hard but
gradually enlarges. Early thyroid cancers are considered as
asymptomatic and are detected incidentally during other examinations
for unrelated medical conditions. Whereas, in more advanced stages,
symptoms may include a palpable neck mass or thyroid nodule.
Due to
the compression of surrounding structures, the patient feel
difficulty in swallowing, called dysphagia, and shortness of breath,
called dyspnoea. Hoarseness while speaking due to nerve involvement
is also a sign of the disease. A radiating pain in the neck to the
jaw or ear can also be present. In advanced stages, symptoms of
distant metastasis may also become evident, depending on the affected
organs.
These
issues can result from tumour growth compressing nearby structures
such as the oesophagus, trachea, or recurrent laryngeal nerve.
Swelling of cervical lymph nodes (lymphadenopathy) is also common.
Less specific symptoms may include facial flushing, softer stools or
diarrhoea, weight loss, and a persistent cough, with some of these
signs being harder to detect on darker skin tones.
Epidemiological Trends
Thyroid
cancer shows a marked predilection for women, with a female to male
ratio 3:1. The peak incidence observed in individuals aged 30–50
years, though medullary and anaplastic thyroid cancers are more
prevalent in older populations. In India, thyroid cancer accounts for
around 2–3% of all cancers, with a notably higher incidence in
coastal areas, possibly due to iodine deficiency or excess. Papillary
carcinoma is the most prevalent subtype, with its incidence are
rising due to advanced diagnostic techniques and imaging technology.
Women in their 30s and 40s are more susceptible to this condition.
Environmental factors, genetic predisposition, and a history of
radiation exposure also play significant roles in its epidemiology.
Risk Factors
Thyroid
cancer can arise from various risk factors, including iodine
deficiency or excess. A family history of thyroid cancer or
associated genetic syndromes, such as Multiple Endocrine Neoplasia
type-2 (MEN2), increases susceptibility, as does the presence of
pre-existing thyroid conditions like goitre or Hashimoto’s
thyroiditis.
Ionising
radiation is a significant risk factor for the development of thyroid
cancer, particularly when exposure occurs during childhood. This is
because the thyroid gland in children is highly sensitive to
radiation-induced damage. Ionising radiation causes direct DNA strand
breaks and specific genetic mutations.
Patterns
of disease spread vary by subtype; papillary thyroid
carcinoma commonly spreads through lymphatic pathways to cervical
lymph nodes, while follicular thyroid carcinoma tends to metastasise
via the bloodstream to distant sites such as the lungs, bones, and
occasionally the brain. In contrast, anaplastic carcinoma exhibits
aggressive local invasion, affecting structures like the trachea and
oesophagus. The most frequent sites of distant metastasis for thyroid
cancer include the lungs, followed by the bones, liver, and, less
commonly, the brain.
Treatment Drawbacks
Surgery
is the most common treatment in allopathic system, where either the
entire thyroid (total thyroidectomy) or part of it (partial
thyroidectomy or lobectomy) is removed. As a result the patient would
be left in traumatic condition for several months that severely
affects their normal life. It also carries risks such as nerve damage
induced voice or swallowing issues, hypoparathyroidism and infection.
If the cancer has spread to nearby lymph nodes, these may also be
removed during the surgical procedure. Thyroid glands are responsible
for regulating calcium levels in the body by producing parathyroid
hormone (PTH). When these glands are surgically removed, it leads to
low calcium levels in the blood, the condition is called
hypocalcaemia and elevated phosphorus levels known as
hyperphosphataemia. As a result, post-surgical period will also be
very complicated, painful and simultaneously expensive to maintain
health.
Post-surgical
hormone therapy is necessary in most cases to replace the hormones
produced by the thyroid and to reduce the risk of cancer recurrence.
Hormone therapy is required lifelong and may cause side effects like
fatigue, weight changes or mood disturbances if not properly
balanced. Patients who have had part of their thyroid removed, may
also require hormone tablets. Despite these procedures recurrence is
not a distant fact.
Radioactive
iodine treatment is another approach, using a small dose of radiation
delivered as a tablet or drink to destroy any remaining cancer cells
after surgery. It aims preventing recurrence or treat metastases. On
the other hand, this method can lead to dry mouth, altered taste,
salivary gland swelling, or, in rare cases, secondary malignancies.
Targeted
medicines are used when other treatments are ineffective or the
cancer has spread, focusing on inhibiting specific processes that
help cancer grow. While compared to other methods targeted therapy
result in significant side effects such as fatigue, hypertension,
diarrhoea, and skin problems.
Chemotherapy,
while not commonly employed for thyroid cancer, may be used in
advanced cases where the cancer has recurred or metastasised. It
reportedly causes to systemic toxicity, including nausea, hair loss,
and immune suppression, sometimes outweighing its benefits in thyroid
cancer management.
In
advanced thyroid cancer cases, complete cure may not be possible
according to allopathic medicine, hence the treatment goal shifts to
managing the disease, alleviating symptoms, and extending life
expectancy after surgical procedures.
Despite
‘advanced’ medical treatments in allopathic system, recurrence
remains a major concern, particularly in aggressive subtypes like
medullary and anaplastic thyroid cancers. Surveillance with regular
imaging and thyroglobulin testing is essential but it can lead to
anxiety disorder and a decreased quality of life. These limitations
highlight the need for a more holistic treatment.
Homoeopathic Approach
Instead
of removing maligned thyroid glands surgically, homoeopathic remedies
revive these glands by enhancing regeneration of healthy cells
followed by strengthening natural healing mechanism of human body.
Since thyroid cancer originate from follicular epithelial cells and
parafollicular C cells, these remedies regulate normal cellular
process within the gland. Homoeopathy emphasises on a holistic
approach rather than treating a symptom of disease. The underlying
bodily imbalances results in the manifestation of cancerous symptoms.
Hence, instead of focusing the symptoms, treating individual as a
whole helps restoring innate immunity for long-term wellbeing.