Uterine Cancer
The uterus, or womb, is a central part of
the female reproductive system. It is a hollow, muscular, pear-shaped organ
where a foetus develops and grows during pregnancy. The lower part of the
uterus, known as the cervix, connects the uterus to the vagina, serving as a
passage between the two. Uterine cancer refers to any malignant tumour that
originates in the uterus.
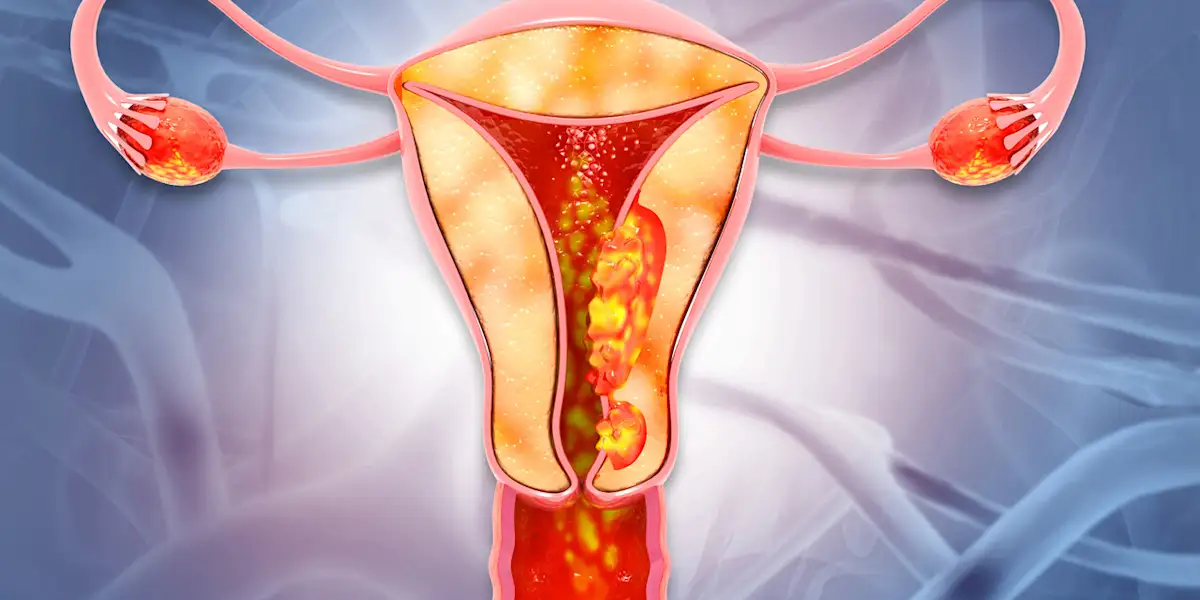
The uterus is divided into two main
sections: the lower end, or cervix, and the upper portion, referred to as the
body or corpus. Structurally, the uterus consists of three distinct layers. The
innermost layer, called the endometrium, is made up of glandular tissue
that lines the uterus and plays a vital role in pregnancy and menstruation.
Surrounding the endometrium is the myometrium, a thick layer of smooth
muscle that facilitates uterine contractions during labour and menstruation.
The outermost layer, the serosa, is a thin tissue coating that protects
the uterus and separates it from surrounding organs.
Changes to cells in the uterus can sometimes
lead to precancerous conditions. This means that the cells appear abnormal but
they are not yet become cancerous. The most common precancerous condition of
the uterus is atypical endometrial hyperplasia. Atypical endometrial hyperplasia
is a condition where the endometrium becomes abnormally thick due to an
overgrowth of the cells lining the uterus. The myometrium has specific
precancerous conditions, such as STUMP and atypical leiomyomas, which can
progress to malignancy. The serosa is primarily a connective tissue layer and
is not as prone to direct malignancy or precancerous changes as glandular or
smooth muscle tissues.
Primarily there are 2 types of uterine
cancer. Most uterine cancers are endometrial carcinoma, which starts from cells
in the lining of the uterus called endometrium. If a carcinoma starts in the
cervix, it is a cervical carcinoma. Carcinomas starting in the endometrium are
endometrial carcinomas. More than 95% of uterine cancers are carcinomas.
Uterine sarcoma develops in the supporting
tissues of the uterus, including muscle, fat, bone and fibrous tissue (material
that forms ligaments and tendons).
A third type of cancer called
carcinosarcoma sometimes develops in the uterus. Another type of cancer that
starts in the uterus is called carcinosarcoma. These cancers start in the
endometrium and have features of both sarcomas and carcinomas. These cancers
were known as malignant mixed mesodermal tumours or malignant mixed mullerian
tumours.
Uterine sarcoma is a rare type of uterine cancer and aggressive group of malignant neoplasm
that arises from the smooth muscle or connective tissue of the uterus called
myometrium. Unlike other forms of uterine cancer, such as endometrial
carcinoma, uterine sarcoma originates in the structural and supportive tissues
of the uterus rather than its lining.
Sarcomas are cancers that start from
tissues like muscle, fat, bone, and fibrous tissue (the material that forms
tendons and ligaments). Cancers that start in epithelial cells, the cells that
line or cover most organs, are called carcinomas.
Various Types of Sarcoma
The below category encompasses a broader range of
uterine sarcomas that can arise from various tissues in the uterus, not just
the endometrial stroma. It includes tumours from different tissue types,
including smooth muscle and mixed tumour types. The tumours are classified
based on their histological features and tissue origin.
1. Leiomyosarcoma:
Originates from the smooth muscle of the uterus called myometrium. Most common
subtype of uterine sarcoma, highly aggressive with a tendency to metastasise,
especially to the lungs.
2. Endometrial
Stromal Sarcoma (ESS): Originates from the connective
tissue of the endometrium or the uterine lining.
3. Undifferentiated
Uterine Sarcoma: A poorly differentiated tumour,
making it difficult to determine its tissue of origin.
4. Adenosarcoma:
A mixed tumour, which contains both glandular (epithelial) and sarcomatous
(connective tissue) components. Typically less aggressive than other uterine
sarcomas, though it can still cause significant health problems.
The World Health
Organization (W.H.O) classifies endometrial stromal neoplasms
into four groups. This arise from the connective tissue of the endometrium.
These tumours are generally classified by differentiation and aggressiveness.
1. Endometrial Stromal Nodule: Benign
tumour that arises from the connective tissue of the endometrium. Does not have
malignant features and does not spread. Generally considered the least
aggressive.
2.
Low-Grade Endometrial Stromal Sarcoma
(LG-ESS): Malignant but slow-growing tumour originating
from the endometrial stroma. Better prognosis due to its slower progression and
lower likelihood of metastasis.
3.
High-Grade Endometrial Stromal Sarcoma
(HG-ESS): A malignant tumour originating from the
endometrial stroma, but with a highly aggressive nature. Characterized by rapid
growth and a higher risk of metastasis.
4. Undifferentiated Uterine Sarcoma: Poorly
differentiated or undifferentiated tumour, making it difficult to determine its
tissue of origin. This is a highly aggressive tumour with poor prognosis.
Both categories share some overlap (like
undifferentiated uterine sarcoma), they focus on different aspects of uterine
sarcomas and employ different criteria for classification.
Trends
Although uterine cancer is the most common
malignancy affecting the female reproductive system, uterine sarcoma accounts
for only a small part of these cases. It is estimated that uterine sarcomas
represent approximately 3 to 5 per cent of all uterine tumours and about 1 per
cent of malignancies affecting the female genital tract. In India, the
incidence of uterine sarcomas is still low compared to endometrial carcinoma,
but trends show a gradual rise in uterine malignancies due to changing
lifestyle factors, hormonal influences, and delayed childbearing. Uterine
sarcoma primarily occurs in postmenopausal women normally around 50-60, with
risk factors including prior pelvic radiation therapy and certain genetic
predispositions.
Method of Metastasis
Uterine sarcoma can be highly aggressive
and metastasising to other parts of the body, such as the lungs, liver, or
bones. This process occurs when cancer cells break away from the primary tumour
in the uterus and travel to distant sites through the bloodstream or lymphatic
system.
Cancer cells grow and invade nearby tissues
within the pelvic area, such as the cervix, bladder, or rectum is referred as local
invasion. If cancer cells enter the lymphatic system, a network of
vessels and nodes that helps fight infections, known as lymphatic spread.
They can travel to nearby or distant lymph nodes. Whereas cancer cells may enter
the bloodstream and can be carried to distant organs, such as the lungs, liver,
or bones is considered as haematogenous spread. Establishing
Secondary Tumours means the cancer cells settle in new locations and
begin to grow, forming secondary tumours.
Common sites of
metastasis
Uterine sarcoma often metastasises to the
lungs, liver, bones, and peritoneal cavity. Once uterine sarcoma spreads to
other parts of the body, it is considered advanced or metastatic cancer. The
prognosis worsens when uterine sarcoma metastasises because it becomes more
difficult to control and treat. Early detection and treatment are crucial to
limit the spread and improve outcomes.
·
The lungs are the most frequent location where
uterine sarcoma spreads, causing symptoms such as shortness of breath or chest
pain.
·
When cancer cells metastasize to the liver, they
may travel through the bloodstream, leading to symptoms like jaundice or
abdominal swelling.
·
Bone metastases can result in severe pain or
fractures due to the formation of secondary tumours in the bones.
·
Additionally, the cancer may spread locally to
the abdominal lining also known as peritoneal cavity, further complicating the
condition.
Risk Factors and Recurrence
Women who have a higher number of menstrual
periods during their lifetime have a greater risk of developing uterine cancer.
Other risk factors include
Ø
Genetic Factors
Ø
Tamoxifen use; for breast cancer treatment, has
a weak oestrogen-like effect on the uterus
Ø
Obesity; excess fat tissue converts androgens
into oestrogens
Ø
Age and Menopause; most cases diagnosed in
postmenopausal women and over 50 years
Ø
Diabetes and Hypertension; Fatigue, weight loss,
and general malaise may indicate metastasis
Uterine sarcomas have an aggressive
clinical behaviour with a tendency to local recurrence and distant spread. The
local recurrence of uterine sarcomas within the pelvis after treatment is high,
even if the initial neoplasm is surgically removed because sarcomas usually
invades surrounding tissues. The recurrence often occurs within 2–3 years of
initial treatment.
Symptoms
The symptoms of uterine sarcoma are often
non-specific and can overlap with other conditions. Both uterine sarcomas and
leiomyomas have similar symptoms. Not all women with these symptoms have
uterine sarcoma, though require medical attention.
v
Most common symptom is irregular vaginal
bleeding, especially in postmenopausal women
v
Unusual, watery, or blood-tinged vaginal
discharge
v
Pelvic and abdominal pain due to tumour or
spread or local recurrence
v
Changes in urinary and bowel habits
v
Palpable mass may be felt in the pelvis or lower
abdomen
v
Fatigue, weight loss, and general malaise may
indicate metastasis
Allopathic Treatment
Uterine cancer treatments in allopathy vary
based on the type, stage, and aggressiveness of the disease. However, uterine
cancer is often treated with surgery and in metastasis cases, particularly
uterine sarcomas, involve more aggressive and sometimes irreversible
treatments. In radical hysterectomy the patient has been undergoing complete removal
of the uterus and surrounding tissues. Similarly, radiation therapy and
chemotherapy can result in significant physical and emotional suffering,
including infertility, persistent hormonal imbalances and chronic pain. Despite
these aggressive treatment methods uterine sarcoma often have high recurrence rates
and poor survival outcomes.
Homoeopathy Remedies for Uterine Cancer
Homoeopathy adopts a different treatment
approach in disease treatment compared to allopathy. Instead of focusing the
disease, homoeopathy takes a holistic approach aiming to stimulate self-healing
capacity of our body. This system of medicine views health as a balance of the
vital force, and any disruption to this balance manifests as disease symptoms.
Therefore, the focus of homoeopathic treatment lies in restoring this balance,
addressing the root cause rather than merely alleviating the symptoms. As a
result, it ensures minimal side effects and encourages the body to recover
naturally.
Homoeopathy also considers the metastasis
condition of uterine cancer uniquely. It believes that treating symptoms alone
may suppress the condition, potentially driving it deeper into the system.
Instead, it aims to eliminate the underlying imbalance to achieve overall
health. By focusing on restoring harmony in the vital force, homoeopathy not
only addresses the disease but also promotes overall health and resilience.
Homoeopathic remedies act at a cellular
level, modifying pathological changes by improving cellular energy dynamics,
reducing oxidative stress and promoting programmed cell death (apoptosis) in
abnormal cells. These effects prevent the unregulated growth of malignant cells
and promote the repair of damaged tissues. The remedies also influence
epigenetic mechanisms, which regulate gene expression without altering the
underlying DNA sequence. By doing so, homoeopathy aims to correct genetic
imbalances that contribute to the progression of cancer.